According to a new study published by the journal Respiratory Research, activation of the body’s cannabinoid-2 receptor ameliorates (makes better) pseudomonas aeruginosa-induced lung injury and inflammation, “thus paving the path for new therapeutic avenues against PA pneumonia.”
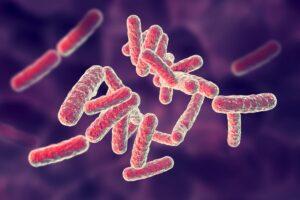
As noted by the study’s abstract, bacterial pneumonia is a major risk factor for acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). Pseudomonas aeruginosa (PA), an opportunistic pathogen with an increasing resistance acquired against multiple drugs, “is one of the main causative agents of ALI and ARDS in diverse clinical settings.”
Given the anti-inflammatory role of the cannabinoid-2 receptor (CB2R), “the effect of CB2R activation in the regulation of PA-induced ALI and inflammation was tested in a mouse model as an alternative to conventional antibiotic therapy.” CB2R activation is done naturally through the consumption of cannabis and cannabinoids.
In order to activate CB2R, a selective synthetic agonist, JWH133 (meant to mimic the effects of natural cannabinoids), was administered intraperitoneally (i.p.) to mice. Furthermore, SR144528 (a selective CB2R antagonist) was administered in combination with JWH133 to test the specificity of the CB2R-mediated effect.
PA was administered intratracheally (i.t.) for induction of pneumonia in mice. At 24 h after PA exposure, lung mechanics were measured and the total cell number, protein content, and neutrophil population in the bronchoalveolar lavage fluid (BALF) were determined. The bacterial load in the whole lung was also measured.
CB2R activation by JWH133 “was found to significantly reduce PA-induced ALI and the bacterial burden.” CB2R activation “also suppressed the PA-induced increase in immune cell infiltration, neutrophil population, and inflammatory cytokines.”
Researchers state that “These effects were abrogated by a CB2R antagonist, SR144528, further confirming the specificity of the CB2R-mediated effects.”
“CB2R-knock out (CB2RKO) mice had a significantly higher level of PA-induced inflammation as compared to that in WT mice”, states researchers. “CB2R activation diminished the excess activation of neutrophils, whereas mice lacking CB2R had elevated neutrophil activation. Pharmacological activation of CB2R significantly reduced the PA-induced NF-κB and NLRP3 inflammasome activation, whereas CB2KO mice had elevated NLRP3 inflammasome.”
Researchers concude: “Our findings indicate that CB2R activation ameliorates PA-induced lung injury and inflammation, thus paving the path for new therapeutic avenues against PA pneumonia.”
Below is the full abstract for the study:
Abstract
Background: Bacterial pneumonia is a major risk factor for acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). Pseudomonas aeruginosa (PA), an opportunistic pathogen with an increasing resistance acquired against multiple drugs, is one of the main causative agents of ALI and ARDS in diverse clinical settings. Given the anti-inflammatory role of the cannabinoid-2 receptor (CB2R), the effect of CB2R activation in the regulation of PA-induced ALI and inflammation was tested in a mouse model as an alternative to conventional antibiotic therapy.
Methods: In order to activate CB2R, a selective synthetic agonist, JWH133, was administered intraperitoneally (i.p.) to C57BL/6J mice. Furthermore, SR144528 (a selective CB2R antagonist) was administered in combination with JWH133 to test the specificity of the CB2R-mediated effect. PA was administered intratracheally (i.t.) for induction of pneumonia in mice. At 24 h after PA exposure, lung mechanics were measured using the FlexiVent system. The total cell number, protein content, and neutrophil population in the bronchoalveolar lavage fluid (BALF) were determined. The bacterial load in the whole lung was also measured. Lung injury was evaluated by histological examination and PA-induced inflammation was assessed by measuring the levels of BALF cytokines and chemokines. Neutrophil activation (examined by immunofluorescence and immunoblot) and PA-induced inflammatory signaling (analyzed by immunoblot) were also studied.
Results: CB2R activation by JWH133 was found to significantly reduce PA-induced ALI and the bacterial burden. CB2R activation also suppressed the PA-induced increase in immune cell infiltration, neutrophil population, and inflammatory cytokines. These effects were abrogated by a CB2R antagonist, SR144528, further confirming the specificity of the CB2R-mediated effects. CB2R-knock out (CB2RKO) mice had a significantly higher level of PA-induced inflammation as compared to that in WT mice. CB2R activation diminished the excess activation of neutrophils, whereas mice lacking CB2R had elevated neutrophil activation. Pharmacological activation of CB2R significantly reduced the PA-induced NF-κB and NLRP3 inflammasome activation, whereas CB2KO mice had elevated NLRP3 inflammasome.
Conclusion: Our findings indicate that CB2R activation ameliorates PA-induced lung injury and inflammation, thus paving the path for new therapeutic avenues against PA pneumonia.